The Importance of Stretch Breaks for Knee Comfort
Maintaining joint comfort, particularly in the knees, is essential for daily mobility and overall quality of life. Stretch breaks throughout the day can play a crucial role in managing osteoarthritis and knee pain by supporting tissue health and improving flexibility. This article explores how structured stretching and strengthening exercises, combined with medical treatments, can enhance joint comfort and function for those living with knee osteoarthritis.
Understanding Knee Osteoarthritis and Its Management
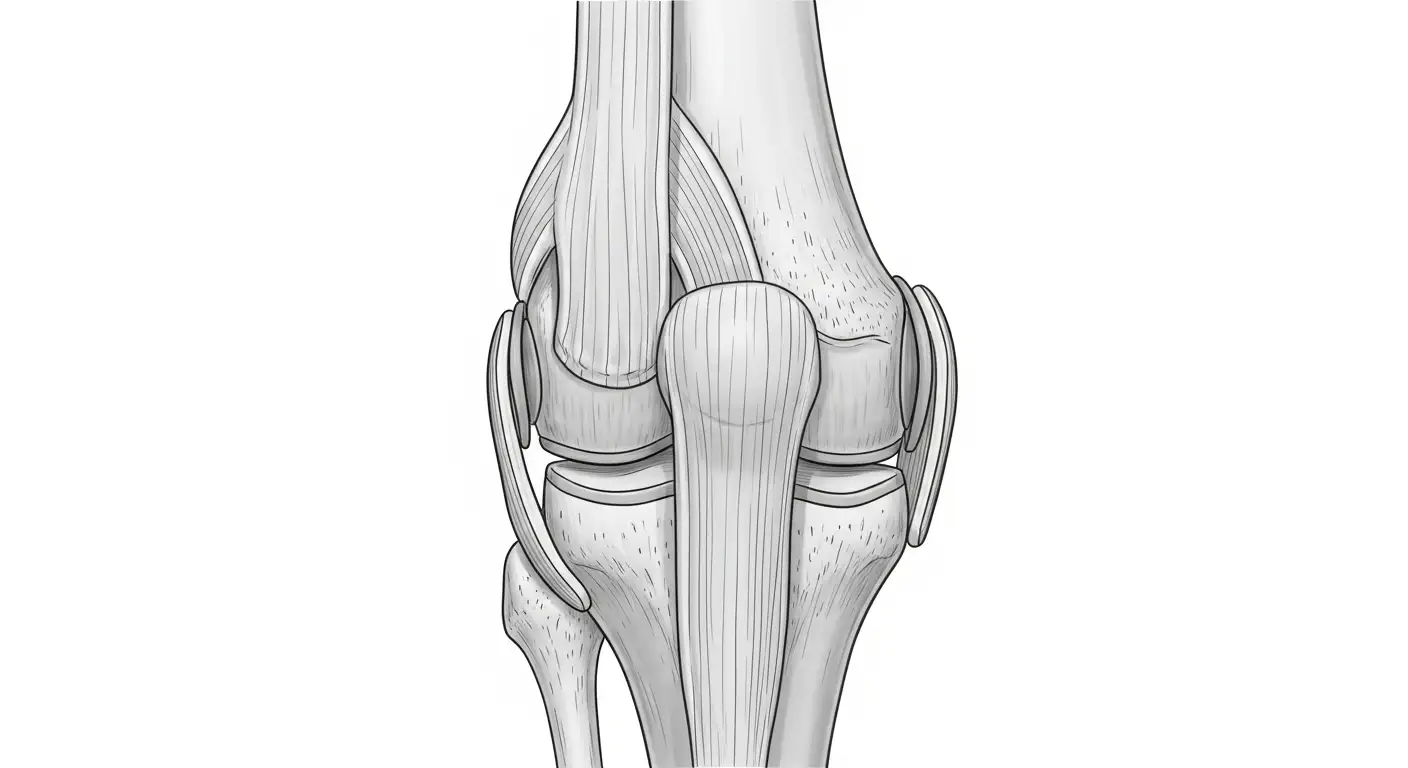
What is Knee Osteoarthritis and Its Impact?
Knee osteoarthritis (OA) is a common joint condition characterized by the gradual degeneration of cartilage in the knee, leading to pain, stiffness, and reduced mobility. This condition affects millions worldwide, impairing daily activities and overall quality of life.
Why is Maintaining Joint Function Important?
Maintaining joint function is essential to prevent further deterioration, preserve independence, and reduce pain. Strengthening muscles around the knee supports the joint by absorbing shocks during movement, while maintaining flexibility helps prevent stiffness and improves range of motion (ROM).
What are Effective Strategies for Managing Knee Osteoarthritis?
Management of knee OA involves a combination of approaches:
- Exercise and Physical Therapy: Low-impact, gentle exercises such as leg raises, hamstring stretches, half squats, and calf raises improve muscle strength and joint flexibility without causing pain or stress.
- Stretching Programs: Regular stretching targeting quadriceps, hamstrings, hip flexors, and calf muscles enhances flexibility, reduces pain, and improves knee joint ROM. Stretching exercises performed 2-3 times daily, holding stretches for 20-30 seconds, have shown significant benefits.
- Monitoring Pain and Exercise Intensity: Using pain ratings (0-3 minimal, 4-5 acceptable, 6-10 excessive) helps guide exercise intensity, ensuring pain does not worsen with activity.
- Medical Treatments: Pharmacological options like NSAIDs and corticosteroid injections reduce inflammation and pain, while surgical options such as total joint replacement may be considered in severe cases.
- Lifestyle Adjustments: Weight management, use of supportive devices, and low-impact aerobic activities like walking, swimming, cycling, yoga, or tai chi reduce joint stress and improve overall function.
Together, these strategies help patients manage symptoms, improve knee function, and maintain an active lifestyle.
The Role of Non-Surgical Interventions in Knee Osteoarthritis
How do non-surgical interventions help manage osteoarthritis-related knee pain?
Non-surgical strategies are essential for managing knee osteoarthritis (OA), focusing on reducing pain and improving joint function without surgery. These interventions include a combination of exercise, weight management, mechanical aids, and pharmacological treatments.
Non-surgical strategies for pain management
Engaging in low-impact, gentle exercises such as walking, swimming, cycling, and yoga helps maintain a full range of motion and strengthens muscles supporting the knee joint. Strengthening exercises targeting the quadriceps, hamstrings, and surrounding muscles can reduce stress on the knee by improving shock absorption. Stretching exercises that improve flexibility of the hamstrings, quadriceps, hip flexors, and calf muscles also reduce knee joint strain and pain.
Mechanical aids like knee braces and foot orthoses help redistribute load away from painful joint areas, providing symptomatic relief and enhancing function. Pharmacological options include NSAIDs and acetaminophen for pain control, corticosteroid injections for flare-ups, and supplements such as glucosamine and chondroitin that may help support cartilage health.
Weight management and muscle strengthening
Maintaining a healthy weight is crucial as excess load increases joint stress and accelerates cartilage breakdown. A combination of weight loss and structured strengthening programs focusing on the quadriceps and hip muscles can improve knee stability and decrease pain intensity.
Exercise programs typically involve gradual increases in repetitions and resistance, with the goal of performing strengthening exercises two to three times weekly. Stretches should be held 20-30 seconds and repeated in multiple sets daily to enhance flexibility and prevent joint contractures.
Mechanical aids and pharmacological options
Alongside exercise and weight management, mechanical aids can be used to modify joint loading biomechanics. Foot orthoses and knee braces are frequently employed to alleviate pain by redistributing pressure.
Pharmacological treatments are useful adjuncts during periods of increased symptoms, helping to control inflammation and pain. For persistent or severe cases, corticosteroid injections may be considered under medical supervision.
Together, these non-surgical interventions provide a comprehensive approach to managing knee osteoarthritis, aiming to reduce pain, improve function, and potentially delay the need for surgical procedures.
Stretching and Strengthening: Foundation for Joint Comfort

Why is maintaining range of motion important for knee osteoarthritis?
Maintaining a full range of motion (ROM) in the knee joint is essential for joint health and comfort, especially in osteoarthritis (OA). Stretching not only enhances flexibility but also reduces joint stiffness and pain. Moderate-quality evidence confirms that stretching can improve total knee ROM by an average of 9.3°, with specific gains in knee flexion and extension. Improved flexibility supports daily activities and helps prevent contractures that limit movement.
Which muscle groups are important to strengthen for knee support?
Strengthening the muscles around the knee helps absorb ground impact and reduces stress on the joint. Critical muscle groups to target include:
- Quadriceps
- Hamstrings
- Hip abductors and adductors
- Gluteal muscles
Strong muscles provide shock absorption and support joint stability, thereby alleviating knee pain and aiding tissue healing.
What are some effective stretching and strengthening exercises?
A comprehensive knee conditioning program incorporates both stretching and strengthening exercises tailored for osteoarthritis management. Examples include:
| Exercise Type | Examples | Purpose |
|---|---|---|
| Stretching | Quadriceps stretch, hamstring stretch, hip flexor stretch, calf stretch | Improve flexibility and reduce joint strain |
| Strengthening | Leg raises, half-squats, hamstring curls, calf raises, hip abduction, leg presses | Build muscle strength to support the knee joint |
Additional activities such as walking, swimming, cycling, yoga, Tai Chi, and balance exercises can complement these routines by enhancing flexibility, balance, and overall joint function. These are generally performed 2–3 times per week, starting with low repetitions (2–3) and gradually increasing to up to 2 sets of 15 reps. Stretches should be held for 20–30 seconds and done multiple times daily.
By regularly practicing these tailored exercises, individuals with knee osteoarthritis can maintain joint mobility, strengthen muscles, and reduce discomfort—supporting a more active and independent lifestyle.
Guidelines for Safe and Effective Stretch Breaks

How to Monitor Exercise Intensity Using Pain Ratings
To maintain safe exercise levels for knee osteoarthritis, use a simple pain rating scale after or during activities. A score of 0-3 indicates minimal pain and is ideal, 4-5 is considered acceptable, but 6-10 means pain is excessive and the exercise intensity should be reduced. Any increase in knee pain during exercise should be short-term and manageable, never worsening or continuing past the session.
How Should You Gradually Increase Exercise Repetitions and Resistance?
Begin with small repetition sets—around 2 to 3 repetitions—and gradually build up to 2 sets of 15 repetitions for strengthening movements. Resistance can be increased slowly as exercises feel easier, ensuring muscles supporting the knee become stronger without aggravating pain. Performing these exercises regularly, about 2-3 times a week, helps maintain strength and mobility.
When Should You Stop Exercises or Seek Professional Advice?
If symptoms worsen or new knee pain develops during stretching or strengthening exercises, stop immediately. Persisting pain beyond 6 weeks, or any worsening despite modifications, warrants consultation with a healthcare professional. Proper form during stretches and exercises is critical to avoid joint strain and injury. Always warm up with low-impact activities, and avoid pushing beyond manageable pain limits to ensure safety and promote healing.
Specific Stretching Techniques to Support Knee Health
Which stretching exercises are most effective for knee osteoarthritis?
To support knee health and manage osteoarthritis symptoms, focus on stretching the hamstrings, quadriceps, hip flexors, and calf muscles. Hamstring stretches such as supine leg raises and seated stretches improve hamstring flexibility, reducing strain on the knee joint. Quadriceps stretches, like the standing quadriceps stretch, help maintain knee joint support and alleviate discomfort. Hip flexor stretches — including kneeling hip flexor exercises — enhance mobility essential for knee function. Calf muscle stretches, for example, standing calf stretches, support walking and movement, which can influence knee comfort.
How long should you hold these stretches and how often should they be done?
Stretching sessions typically involve holding each stretch for 20 to 30 seconds, performing 2 to 3 sets per session. Repeating stretches 2 to 3 times daily can effectively improve range of motion and flexibility. Evidence suggests static stretching accumulated for 10 minutes weekly or performed in multiple short sessions yields beneficial flexibility gains.
What is proper form and how can injury be prevented during stretching?
Maintaining proper form during stretching is critical to avoid joint strain. Perform gentle, slow stretches with controlled breathing and a proper warm-up, such as low-impact activities like walking or stationary biking. Avoid bouncing or forcing stretches; movements should be pain-free and gentle. Stretches done with good form reduce risk of injury and inflammation. Cease exercising immediately if symptoms worsen or new pain arises, and consult a healthcare professional if necessary.
Regularly performing these targeted stretches with attention to timing, frequency, and form can improve knee flexibility, reduce pain, and support better function in individuals managing knee osteoarthritis.
The Benefits of Regular Stretching on Knee Mobility and Pain Reduction
How does stretching improve range of motion in knee osteoarthritis?
Research shows that regular stretching leads to significant improvements in knee joint range of motion (ROM) for those with osteoarthritis. Specifically, stretching programs have demonstrated an average total ROM increase of 9.3°, including improvements in both knee flexion by about 10.8° and knee extension by 9.1°. These gains help patients regain mobility, which is crucial for daily activities and overall joint health.
What impact does stretching have on knee pain?
Stretching is also linked to notable pain reduction. Moderate-quality evidence indicates that patients experience a substantial decrease in knee pain, quantified by a standardized mean difference of 1.9 in pain scores. This suggests that beyond mobility, stretching exercises can effectively alleviate discomfort and improve quality of life.
Why is maintaining a consistent stretching routine important?
Consistency is essential to maximize benefits. Performing stretches regularly, ideally 2-3 times per day and holding each stretch for 20-30 seconds across multiple sets, supports lasting flexibility gains. Stretching at the end of exercise sessions as part of a cool-down helps preserve flexibility over time. For best results, incorporating a variety of stretches targeting quadriceps, hamstrings, hip flexors, and calf muscles is recommended.
Together, these exercise practices not only enhance joint function and reduce pain but also serve as a safe, cost-effective strategy to manage knee osteoarthritis conservatively and possibly delay surgical interventions.
Integrating Low-Impact Activities and Variety for Joint Health
Which low-impact activities help manage knee osteoarthritis effectively?
Low-impact exercises such as walking, swimming, cycling, yoga, and tai chi are highly recommended for individuals with knee osteoarthritis. These activities enhance joint movement and muscle strength without imposing excessive stress on the knee. Swimming and cycling provide cardiovascular benefits while reducing joint strain. Yoga and tai chi offer gentle stretching and balance training, which can alleviate arthritis pain and improve overall mobility.
How can balance and flexibility exercises reduce fall risk in those with joint pain?
Incorporating balance and flexibility routines, including lunges, lateral side stretches, and knee-to-chest stretches, plays a vital role in reducing the risk of falls among people suffering from joint pain. Improved flexibility lessens joint stiffness, while better balance helps maintain stability during daily activities. This combination decreases the likelihood of falls and fractures, especially in older adults managing osteoarthritis.
What benefits does engaging in social and outdoor activities have for arthritis sufferers?
Introducing variety through social and outdoor activities can greatly increase adherence to exercise programs. Enjoying movement with others or in nature boosts motivation and enjoyment, which are essential for consistent physical activity. This approach not only supports physical health by enhancing strength and flexibility but also promotes mental well-being, which is crucial for coping with chronic conditions like knee osteoarthritis.
When to Consider Advanced Medical Treatments for Knee Osteoarthritis
What role do injections like corticosteroids and hyaluronic acid play in treating knee osteoarthritis?
Injections such as corticosteroids and hyaluronic acid are often used to ease the symptoms of knee osteoarthritis. Corticosteroid injections help by reducing inflammation, providing short-term pain relief. However, long-term use may risk cartilage damage and hasten joint wear.
Hyaluronic acid injections, on the other hand, work by lubricating the joint to improve mobility and potentially slow the progression of osteoarthritis. They tend to provide longer-lasting relief and carry fewer side effects compared to corticosteroids. Both types of injections are minimally invasive options that aim to relieve pain and improve knee function, yet they are most effective when combined with other treatments.
When is knee replacement surgery considered as a treatment option for osteoarthritis?
Knee replacement surgery is typically considered after conservative treatments—like medications, physical therapy, and injections—fail to adequately manage symptoms for at least six months. It is usually recommended for patients experiencing severe, persistent pain that disrupts daily activities, sleep, or limits walking distance.
Additional signs indicating the need for surgery include joint deformity, limited range of motion, swelling unresponsive to treatments, and a diminished quality of life. Surgery aims to relieve pain and restore mobility when other options no longer suffice, taking into account cartilage damage and overall patient health.
Are there any emerging or innovative therapies for managing knee pain and osteoarthritis?
New treatments are emerging to address knee osteoarthritis beyond the traditional options. One such therapy is genicular artery embolization (knee embolization), a minimally invasive procedure that blocks problematic blood flow to reduce joint inflammation and pain.
Other promising approaches include platelet-rich plasma (PRP) injections, stem cell therapies, and gene therapy, particularly therapies that deliver anti-inflammatory genes directly to the joint. While these methods show potential to regenerate cartilage and modulate inflammation, more research is needed to establish their long-term benefits.
Overall, these advanced therapies offer hope for patients who are not candidates for surgery or who seek alternatives to conventional treatments.
Consultation and Personalized Care: Keys to Long-Term Joint Health

Why Consult Healthcare Professionals Before Starting Exercises?
Before beginning any exercise routine for knee osteoarthritis, consulting a healthcare professional is crucial. They help tailor exercises to your unique condition, ensuring safety and effectiveness. Personalized guidance is especially important to avoid exacerbating pain or causing injury.
How Can You Monitor Symptoms and Adjust Your Exercise Routine?
Monitoring knee pain using a simple rating scale from 0 to 10 helps manage exercise intensity. Ratings from 0-3 indicate minimal pain, 4-5 are acceptable, and 6-10 signal excessive pain. If pain worsens or new symptoms appear, stop exercising and consult your healthcare provider. Gradually increasing repetitions and resistance while listening to your body helps prevent overexertion.
What Role Do Physiotherapists and Orthopedists Play?
Physiotherapists design structured knee conditioning programs focusing on strengthening muscles like quadriceps, hamstrings, and gluteals, as well as stretching exercises to improve range of motion and relieve pain. Orthopedists provide medical assessment, recommend treatments, and may consider interventions like physical therapy or surgery if necessary. This collaborative approach supports long-term joint health and improved quality of life for those managing knee osteoarthritis.
The Path to Sustained Joint Comfort and Mobility
Incorporating regular stretch breaks and targeted exercises into daily routines offers significant benefits for improving knee joint comfort and function, particularly for individuals managing osteoarthritis. These non-surgical strategies, supported by evidence-based practices, help maintain flexibility, reduce pain, and enhance muscle strength to support joint stability. While medical treatments including medications and injections have important roles, a comprehensive approach that includes gentle stretching, strengthening, and professional guidance ensures optimal outcomes. Staying attentive to pain signals, gradually progressing exercise intensity, and seeking personalized care form the foundation for sustaining mobility and quality of life with healthy knees.
References
- Exercises to help with osteoarthritis of the knee
- Knee Conditioning Program - OrthoInfo - AAOS
- Knee Stretches - Arthritis-health
- Five Tips for Safe Stretching to Manage Joint Pain
- Stretching, Bracing, and Devices for the Treatment of ...
- At-home Exercises for Knee Arthritis
- Knee joint replacement - series—Indications
- Total Knee Replacement - OrthoInfo - AAOS
- 8 Signs You May Need a Knee Replacement
- Non-surgical Treatments for Knee Osteoarthritis at ...