Understanding the Vital Role of Follow-Up Care in Knee Health
Knee conditions, whether injuries or degenerative diseases, require careful management and ongoing attention to ensure successful recovery and to maintain long-term joint health. Follow-up care plays an essential role in monitoring healing, preventing complications, and optimizing outcomes, especially after surgical procedures like knee replacement. This article explores the critical aspects of follow-up care, its impact on patient satisfaction, and strategies for lifelong knee health.
Monitoring Healing and Detecting Complications Early

Why is follow-up care important in knee condition recovery and long-term health?
Follow-up care plays a vital role in ensuring optimal recovery after knee surgery or injury. It allows healthcare professionals to closely monitor the healing process, identify early signs of issues like infections, inflammation, or implant problems, and adjust treatment plans accordingly. During these visits, doctors assess pain levels, evaluate physical therapy progress, and check the function of knee implants, contributing to long-term joint health.
Regular follow-up appointments also offer opportunities to review imaging tests such as X-rays or MRIs, which help visualize the internal condition of the knee. These tests are crucial for detecting any underlying problems like implant loosening or abnormal alignment before they develop into more severe complications.
Why is ongoing medical supervision essential for maintaining knee health following procedures like knee replacement or injury?
Continued medical oversight after knee surgeries or injuries is necessary for multiple reasons. It ensures the healing process progresses smoothly, guides patients through appropriate rehabilitation routines, and helps manage pain effectively. Supervision also facilitates early detection of potential complications such as blood clots, infections, or implant failures.
Through regular check-ups, doctors can monitor functional outcomes, adjust medications if needed, and recommend activity modifications to prevent re-injury. This holistic oversight supports a smoother recovery journey, reduces the risk of long-term issues, and enhances the durability of the knee replacement or repair.
What does follow-up care involve?
Follow-up involves scheduled visits where doctors evaluate the knee’s healing status through physical assessment and imaging tests. These appointments enable timely intervention if problems are identified. They also serve as educational sessions, during which patients receive advice on ongoing care, lifestyle modifications, and safe activity levels to support long-term health.
In summary, diligent follow-up care, including regular evaluations and imaging tests, as well as personalised treatment adjustments, are fundamental for successful recovery and maintaining knee health in the years following initial treatment.
Optimizing Recovery Through Personalized Follow-Up Plans
What factors influence the long-term outcomes and patient satisfaction regarding follow-up care for knee conditions?
Long-term success and patient satisfaction after knee treatment are affected by multiple factors. Patient adherence to scheduled follow-up appointments, lifestyle choices such as maintaining a healthy weight, and their psychological attitude toward recovery all contribute significantly.
Biological elements also play a role. These include age, body mass index (BMI), bone density, and the presence of comorbidities like diabetes or arthritis. Pre-existing conditions, especially those affecting mobility or causing pain, can influence recovery trajectories.
Effective postoperative pain management, early mobilization, and consistent participation in physical therapy sessions are vital for achieving optimal results. Preventing complications such as knee stiffness, infections, and blood clots is crucial.
Moreover, social support networks, personalized care plans that consider individual needs, and environmental or cultural factors can substantially enhance patient satisfaction and ensure a smoother long-term recovery.
What role does patient education play in the recovery process from knee injuries or surgeries?
Patient education is a cornerstone of effective recovery. It empowers individuals, helping them understand the importance of following prescribed physical therapy exercises, activity modifications, and medication protocols.
Through education, patients learn how to manage pain, perform strengthening and stretching routines safely, and recognize signs of complications that require medical attention.
This knowledge encourages adherence to rehabilitation programs, reduces anxiety about the recovery process, and enables patients to take an active role in their healing. Education also prepares patients for specific procedures like surgeries or knee replacements, including preoperative preparations and postoperative care.
Ultimately, well-informed patients tend to experience better outcomes, fewer setbacks, and higher satisfaction levels, ensuring the greatest possible restoration of knee function and quality of life.
Factors influencing long-term outcomes following knee surgery
| Factor | Impact | Additional Details |
|---|---|---|
| Follow-up adherence | High adherence correlates with better outcomes | Regular check-ins help catch issues early |
| Lifestyle modifications | Weight management improves joint stress | Reduced strain on the knee aids healing |
| Psychological readiness | Optimism and motivation support recovery | Affects participation in rehab activities |
| Biological factors | Age, BMI, health conditions influence healing | Younger, healthier patients often recover faster |
| Pain management | Effective relief increases activity levels | Improved pain control leads to more movement |
| Social support | Encourages adherence and morale | Family, friends aid in motivation and care |
| Personalized care | Tailored programs improve outcomes | Adjusted rehab based on individual needs |
Understanding these variables allows healthcare providers to craft personalized follow-up strategies. This ensures that each patient's unique circumstances are addressed, promoting better recovery experiences and longer-lasting results.
The Far-Reaching Impact of Postoperative Care on Recovery Success

How does postoperative care, including managing pain and regaining mobility, influence the success of knee surgery recovery?
Postoperative care is fundamental to achieving a successful recovery after knee surgery. Effective pain management, through medications, ice packs, elevation, and movement exercises like ankle pumps, helps reduce discomfort and prevent complications such as blood clots. Proper pain control allows patients to participate actively in physical therapy, which is critical for restoring mobility and joint function.
Gradually increasing activity levels under medical guidance supports tissue healing and enhances strength. Following wound care instructions and activity restrictions minimizes the risk of infection and implant issues. Regular follow-up appointments enable surgeons to monitor progress with evaluations and imaging, ensuring early detection of potential problems. Together, these measures optimize pain relief, promote mobility, and improve the overall outcome of the surgery.
In essence, attentive postoperative care ensures that patients recover smoothly, regain independence quicker, and enjoy improved quality of life post-surgery.
Ultrasound for Patient Comfort and Care Monitoring
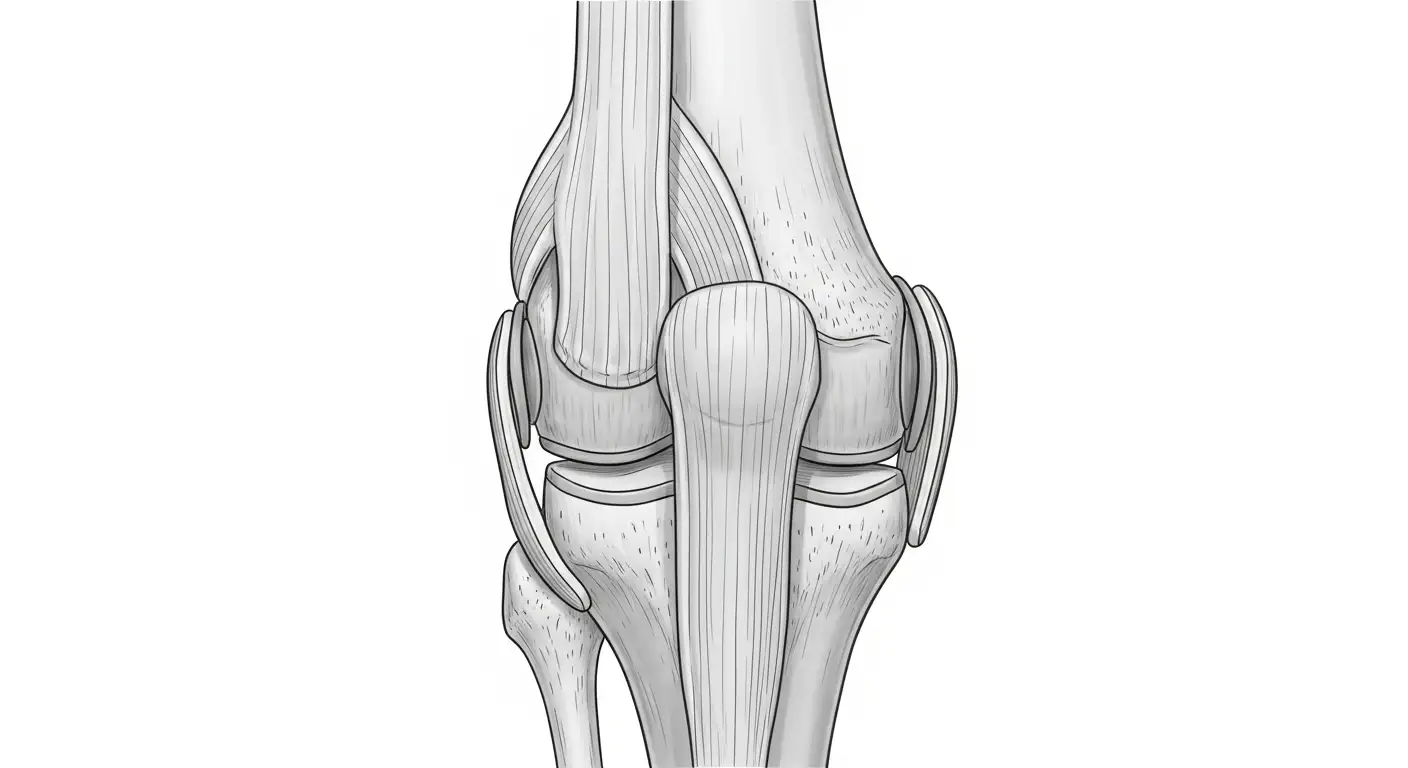
 Follow-up care plays a crucial role in the recovery of knee conditions, especially after surgery or injury. Ultrasound imaging is increasingly used during follow-up visits because it provides real-time visualization of soft tissues surrounding the knee, such as muscles, tendons, and ligaments. This non-invasive technique allows healthcare providers to monitor the healing process closely.
Follow-up care plays a crucial role in the recovery of knee conditions, especially after surgery or injury. Ultrasound imaging is increasingly used during follow-up visits because it provides real-time visualization of soft tissues surrounding the knee, such as muscles, tendons, and ligaments. This non-invasive technique allows healthcare providers to monitor the healing process closely.
One of the main advantages of ultrasound during follow-up is guidance during physical therapy and injections. It helps ensure that therapies target the correct tissue, improving effectiveness and reducing discomfort. Ultrasound can also be used to accurately guide injections of corticosteroids or hyaluronic acid to relieve pain and inflammation when needed.
Monitoring soft tissue healing via ultrasound allows clinicians to detect issues like fluid accumulation, tissue inflammation, or small tears early. This early detection helps prevent complications such as infections or prolonged inflammation from worsening.
The importance of follow-up care extends beyond merely observing healing. Regular check-ups enable adjustments to rehabilitation regimens, medications, or activity levels to optimize recovery. Patient education on maintaining joint health, lifestyle changes, and long-term knee care also takes place during these visits.
In summary, ultrasound imaging enhances follow-up care by providing detailed, real-time evaluation of soft tissue healing, guiding treatments, and allowing early intervention in case of complications. This approach promotes smoother recovery processes, improved patient comfort, and better long-term outcomes.
A variety of factors influence the success of follow-up care, including personalized treatment plans and consistent monitoring. Ultimately, ongoing supervision, often supported by ultrasound imaging, helps ensure that patients regain optimal knee function and avoid future issues, reinforcing the importance of dedicated follow-up for long-term knee health.
Activities of Daily Living and Returning to Function
Walking and mobility milestones
After knee replacement surgery, most patients expect a steady improvement in their walking ability. Initially, using assistive devices like walkers or canes is common, and patients are encouraged to start walking as soon as possible, often on the day of or the day after surgery. The goal is to gradually wean off aids as strength and confidence improve.
Typically, within a few weeks, many patients can walk unassisted. By around 3 months, significant mobility gains are usually observed, and patients often regain the ability to perform daily activities comfortably. Full recovery to maximum strength and endurance generally takes between 6 months to a year, depending on individual factors such as preoperative fitness, age, and overall health.
Resuming household chores and social activities
Restoring independence is a major focus during knee recovery. Patients often resume light household chores — like cooking, cleaning, or shopping — within a few weeks, once they have regained sufficient strength and balance. Social activities, such as visiting friends or engaging in hobbies, are gradually reintroduced as pain diminishes and mobility improves.
Encouragement from physical and occupational therapists, along with support from family and friends, helps ease this transition. It is essential to listen to the body and avoid overexertion early in the recovery process.
Functional movements like kneeling and squatting
Activities involving kneeling and squatting are often more challenging after knee surgery. Many patients have modified their activities preoperatively due to prolonged pain, and some may find these movements less critical for their daily routines.
While some individuals aim to regain full flexibility in these movements, others accept limited range of motion as part of their post-surgical outcome. For those wanting to kneel or squat, specific physiotherapy exercises can be incorporated into recovery programs.
Overall, the importance placed on these movements varies among patients. It is crucial for patients to discuss their activity goals with their surgeon and physical therapist to tailor rehabilitation accordingly.
| Aspect | Typical Timeline | Additional Notes |
|---|---|---|
| Walking independently | Within a few weeks | Use of assistive devices initially, gradual weaning needed |
| Returning to household chores | 2-4 weeks | Based on pain tolerance and strength |
| Resuming social activities | 1-3 months | Adjust according to personal comfort |
| Kneeling and squatting | 3-12 months | Variable based on individual progress and goals |
Understanding these milestones and individual variability helps patients set realistic expectations and stay motivated during their recovery journey.
Rehabilitation and Lifestyle Modifications for Long-Term Knee Health
What factors influence the long-term outcomes and patient satisfaction regarding follow-up care for knee conditions?
Many elements contribute to the success of long-term knee health and patient satisfaction after treatment. Adherence to regular follow-up appointments ensures ongoing monitoring of healing progress, early detection of issues, and timely adjustments to therapy or medications.
Patient behaviors such as maintaining a healthy weight and following medical advice positively impact overall outcomes. Psychological factors, including readiness and motivation, also play crucial roles in recovery.
Biological factors like body mass index (BMI), age, bone density, and existing health conditions such as arthritis influence how well a patient recovers.
Effective pain management, early mobilization, and ongoing physical therapy help prevent complications like stiffness or re-injury. Moreover, social support, personalized care plans, and understanding cultural or environmental influences can heighten satisfaction and improve recovery results.
What are the recommended lifestyle changes to promote long-term knee health and prevent future problems?
To support long-lasting knee health, patients should adopt several lifestyle modifications. Weight management is essential; losing excess weight reduces stress on the knee joints and can slow degeneration.
Engaging in low-impact exercises such as swimming, cycling, and water aerobics helps maintain joint mobility and strength without overloading the knee.
Following an anti-inflammatory diet, like the Mediterranean diet, may reduce joint inflammation and pain. Consuming nutritious foods rich in omega-3 fatty acids, antioxidants, and adequate protein supports tissue repair.
Strengthening routines targeting quadriceps, hamstrings, and core muscles stabilize the knee and improve overall function.
Proper footwear and avoiding high-impact sports or activities that cause joint stress help prevent future injuries.
Prompt medical attention for persistent symptoms and adherence to preventive strategies—like wearing supportive braces or using assistive devices—prolongs the lifespan of the knee and decreases the risk of osteoarthritis progression.
| Aspect | Recommended Practice | Additional Details |
|---|---|---|
| Weight management | Maintain healthy weight | Even modest weight loss significantly benefits knee health |
| Exercise routines | Low-impact activities | Swimming, cycling, water aerobics |
| Diet | Anti-inflammatory diet | Mediterranean diet rich in healthy fats and antioxidants |
| Supportive measures | Proper footwear | Should have good arch support and shock absorption |
| When to see a doctor | Persistent or worsening symptoms | Early intervention prevents further damage |
By integrating these modifications into daily life, patients can enhance their knee joint longevity, reduce pain, and improve overall mobility and quality of life.
Managing Expectations and Building Confidence in Recovery

Addressing fears of re-injury and complications
Many patients worry about re-injury or complications after knee surgery. Understanding the artificial joint or repaired tissue helps in setting realistic expectations. Patients should know that most knee replacements and repairs are successful, with serious complications being infrequent (1-5%). Common concerns include implant loosening, infection, blood clots, or stiffness.
To alleviate fears, it’s important to follow a structured follow-up care plan. Regular check-ups allow healthcare providers to monitor healing, assess implant stability, and catch issues early. Using mobility aids like walkers or canes during initial recovery also provides safety and confidence in moving around.
In case of persistent pain, swelling, or unusual symptoms, early consultation with the surgeon can prevent minor problems from escalating. Education about safe activity levels and avoidance of high-impact movements until fully healed is crucial.
Understanding the artificial joint or repaired tissue
Knowing how an artificial knee works or how repaired tissues heal can support patient confidence. A knee implant typically involves components that mimic natural joint movements. During follow-up visits, surgeons evaluate the implant's position, alignment, and function through physical exams and imaging tests such as X-rays.
Patients are often encouraged to engage in physical therapy to restore strength and mobility. This process gradually shifts focus from protecting the joint to actively regaining function.
For tissue repairs, understanding the healing timeline — usually 6 months for full recovery — emphasizes patience and careful adherence to rehabilitation protocols. With proper care, the joint can provide pain relief and improved mobility for many years.
Patient perceptions and lifestyle adjustments
Patients’ perceptions of their recovery journey greatly influence overall satisfaction. Many adjust daily routines to protect their knees, such as avoiding kneeling or high-impact activities.
Lifestyle modifications include weight management, adopting low-impact exercises like swimming, and following prescribed activity restrictions. Maintaining a positive outlook, staying socially connected, and engaging in hobbies can bolster mental well-being.
Healthcare teams emphasize individualized recovery plans tailored to each patient’s age, activity level, and health status. An understanding of the recovery process fosters patience and resilience, helping patients rebuild confidence linked to regained independence and mobility.
Factors influencing long-term outcomes and satisfaction
Multiple factors influence how well patients recover and how satisfied they are with follow-up care. Adherence to follow-up schedules, maintaining a healthy weight, and following rehab protocols are crucial.
Personal health variables like BMI, age, and comorbidities matter. Patients with good social support and positive attitudes tend to have better outcomes.
Good management of postoperative pain, early mobilization, and prevention of complications such as stiffness or infections directly impact long-term satisfaction. Moreover, cultural and environmental factors, along with thorough patient education, play vital roles.
Why ongoing medical supervision is essential
Continued medical oversight post-surgery ensures optimal joint health. Regular follow-ups help detect issues like implant wear, loosening, or infections early.
Healthcare professionals guide patients through customized rehabilitation programs, advise on safe activity adjustments, and monitor for potential complications. This ongoing supervision not only supports physical recovery but also reassures patients, reinforcing their confidence in long-term joint health.
In summary, proactive follow-up care, patient education, and personalized management strategies are fundamental for successful knee recovery. They help patients regain mobility, reduce fears, and maintain a good quality of life over the years.
Ensuring Long-Term Knee Well-Being through Persistent Care
Effective follow-up care and ongoing medical supervision are indispensable components of successful knee condition management. These processes facilitate early detection of problems, tailored rehabilitation efforts, and lifestyle adjustments that collectively enhance patient satisfaction and long-term outcomes. Patients, healthcare providers, and caregivers must collaborate to prioritize regular check-ups, education, and personalized treatment plans. Building awareness of the critical nature of follow-up not only accelerates recovery but also preserves joint function and quality of life for years to come.
References
- The Importance of Follow-Up Care After Knee Replacement
- Knee Replacement Aftercare: Tips for Patients and ...
- What's important for recovery after a total knee replacement ...
- The Importance of Follow-Up Care After an Orthopedic Injury
- Patient-reported factors determining long-term follow-up ...
- Knee Replacement Recovery FAQs
- How to Maintain Joint Health as You Get Older