The Mystery Behind Popping Knees
Many people experience popping or cracking sounds in their knees without accompanying pain. While these noises can be concerning, they are often harmless. This article explores what it means when your knees pop but don’t hurt, the underlying causes, and when these sounds might signal a more serious issue like osteoarthritis or injury. We also discuss current treatment options and emerging therapies for knee health.
Why Do Knees Pop? The Science Behind the Noise
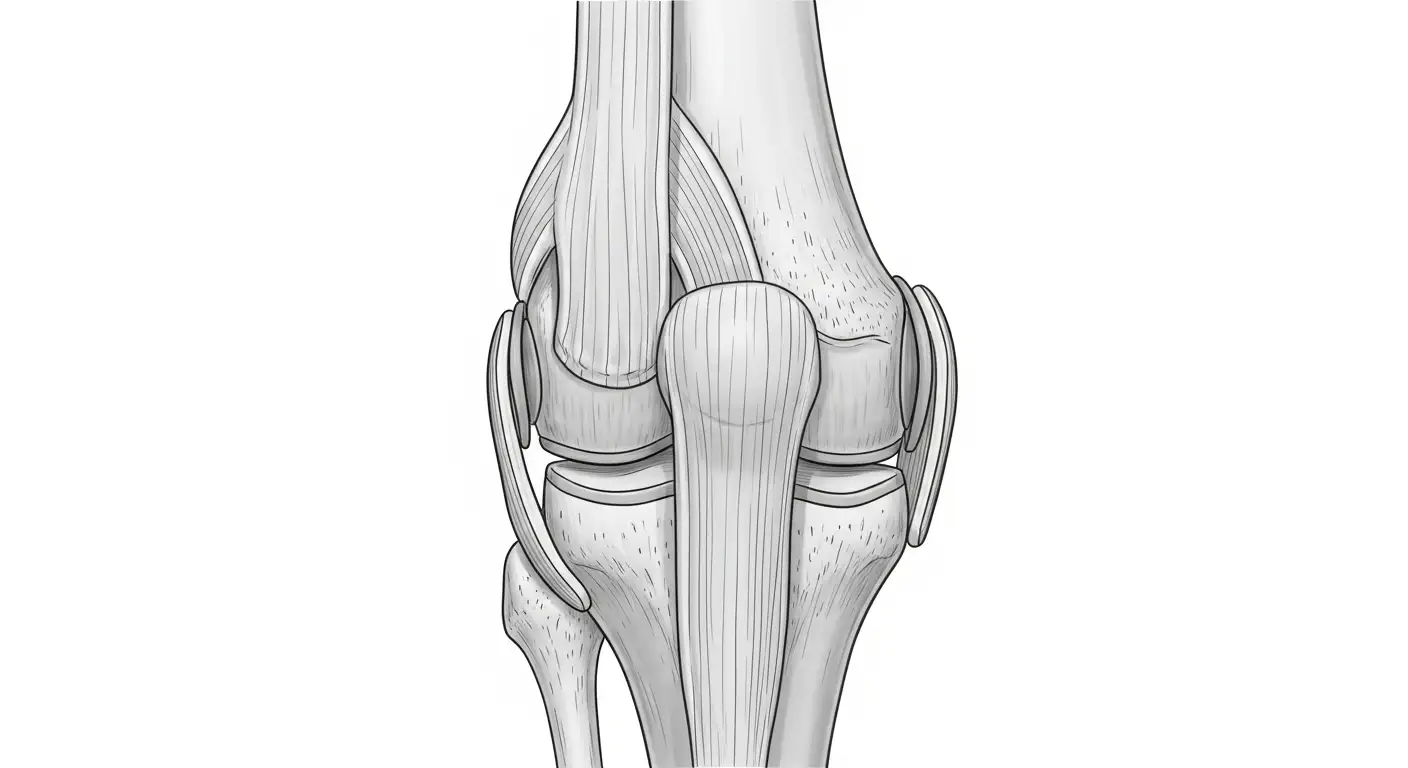
What is Knee Crepitus?
Knee crepitus refers to the popping, cracking, or grinding sounds heard from the knee joint during movement. These noises are quite common and often occur without any accompanying pain.
What Causes the Popping Sound in Knees Without Pain?
Knee popping without pain is usually due to harmless physiological phenomena. The most common cause is the collapse or bursting of tiny gas bubbles within the synovial fluid inside the joint, a process known as cavitation. This sudden release of gas produces the characteristic cracking or popping noise.
How Do Ligaments and Tendons Contribute?
Ligaments and tendons moving or snapping over bony structures can also create popping sounds. For example, as these soft tissues stretch or shift position during knee movement, they may flick or snap back, causing a clicking noise. This is normal and typically does not indicate any damage.
What Are Common Benign Anatomical Contributors?
Certain anatomical features often cause harmless noises in the knee. One example is the plica, a fold in the knee capsule tissue, which can cause clicking or catching sensations without pain. Another is the iliotibial (IT) band, which can snap over the lateral femoral condyle, frequently producing a snapping sound when the knee is in motion.
In summary, most knee popping sounds originate from benign physiological sources like gas bubble cavitation or soft tissue movements, and do not signify any underlying joint problems if pain or swelling are absent.
When Popping Signals Trouble: Pathological Causes and Osteoarthritis
What does popping accompanied by pain indicate?
Popping sounds in the knee that come with pain, swelling, instability, or difficulty moving often signal an underlying problem rather than a harmless noise. Such symptoms may be caused by various knee injuries or degenerative conditions requiring diagnosis and treatment.
Pathological causes of knee crepitus
Pathological crepitus in the knee involves joint noises linked to structural abnormalities or injury. This includes cartilage wear from osteoarthritis (OA), ligament tears (such as ACL, MCL), meniscus tears, tendon ruptures, and conditions like plica syndrome or loose bodies inside the joint. Baker's cyst ruptures and patella subluxation also produce painful popping or snapping sensations with swelling and possible instability.
Relation between crepitus and osteoarthritis
In osteoarthritis, the gradual breakdown of cartilage causes bones to rub together, creating friction and a grinding or cracking noise known as crepitus. Studies show crepitus is a strong predictor of developing symptomatic knee OA. Individuals experiencing frequent crepitus have a significantly increased risk of OA progression, especially if X-rays already show joint disease.
Other knee injuries causing popping with pain
Apart from OA, ligament injuries like ACL tears produce sudden popping sounds accompanied by swelling and instability. Meniscus tears, common after twisting injuries or in older adults, cause clicking, locking, pain, and swelling. MCL injuries involve valgus force mechanisms and generally heal with rest. Tendon tears and patellar dislocations can also present with painful popping and functional impairment.
Signs of knee osteoarthritis relevant to popping
When crepitus hints at OA, it is often associated with other symptoms like knee pain, stiffness, swelling, limited range of motion, muscle weakness, and episodes of instability or buckling. These symptoms reflect the underlying joint degeneration and guide the need for evaluation and management.
Regular checkups, including physical exams and imaging, help assess the severity and cause of popping. Early recognition and treatment can improve knee function, reduce symptoms, and slow disease progression.
Knee Osteoarthritis: Understanding the Condition and Its Symptoms
What is the degenerative nature of osteoarthritis?
Osteoarthritis (OA) of the knee is a long-term, progressive condition where the protective cartilage that cushions the ends of the bones gradually wears away. As this cartilage deteriorates, bones begin to rub against each other, causing friction and inflammation. This leads to symptoms such as pain, swelling, and the characteristic cracking or grinding sounds known as crepitus.
What are the common symptoms of knee osteoarthritis?
Individuals with knee OA often experience a combination of symptoms including:
- Joint pain and aching
- Stiffness, especially after inactivity
- Swelling due to inflammation
- Limited range of motion
- Muscle weakness around the knee
- Crepitus, the popping or grinding noises during movement
- Joint instability or buckling sensations
These symptoms can interfere with daily activities and mobility.
What are the stages of knee osteoarthritis?
Knee OA progresses through four stages, each reflecting the severity of cartilage loss and symptom intensity:
| Stage | Description | Symptoms |
|---|---|---|
| 1 (Minor) | Early cartilage softening and minor bone changes | Mild or no symptoms, slight discomfort |
| 2 (Mild) | Cartilage wears down, early bone spurs develop | Noticeable pain and stiffness, occasional crepitus |
| 3 (Moderate) | Significant cartilage loss, more bone spurs, joint space narrowing | Increased pain, swelling, stiffness, and crepitus |
| 4 (Severe) | Severe cartilage loss with bone-on-bone contact | Chronic pain, joint instability, frequent swelling, limited motion |
What complications can arise from knee osteoarthritis?
Alongside joint pain and stiffness, osteoarthritis can lead to several complications, including:
- Bone spurs (osteophytes): Extra bone growths that may worsen pain and restrict movement.
- Joint instability: Weakening of muscles and ligaments causing wobbliness or buckling.
- Baker's cysts: Fluid-filled sacs behind the knee resulting from joint inflammation.
- Mood disorders: Chronic pain and disability can contribute to anxiety and depression.
Understanding these symptoms and stages helps guide appropriate management and treatment to maintain knee function and quality of life.
Diagnosing Knee Problems Associated with Popping: What to Expect
Clinical Assessment of Popping Knees
When you visit a healthcare provider for knee popping, the initial step involves discussing your symptoms in detail. The clinician will inquire if the popping is accompanied by pain, swelling, instability, or difficulty in movement, which could suggest underlying pathology such as osteoarthritis or ligament injury. Patterns of popping, frequency, and associated activities are also important for diagnosis.
Physical Examination Components
A thorough physical examination is performed to assess key elements of knee health. This includes checking for swelling, tenderness, range of motion, and stability of the knee joint. The doctor may look for muscle weakness or joint instability and listen for characteristic sounds like crepitus during motion. Gait and limb alignment are also evaluated to identify mechanical issues contributing to symptoms.
Imaging Techniques such as X-ray, MRI, and Ultrasound
Imaging plays a crucial role in diagnosis. X-rays can reveal bone spurs, joint space narrowing, or other osteoarthritis signs. MRI provides detailed views of soft tissues like ligaments, menisci, and cartilage, detecting tears or degeneration. Diagnostic ultrasound is useful for dynamic assessment of tendons, ligaments, and fluid collections and can identify issues such as plica syndrome or Baker's cyst.
Differentiating Physiological vs. Pathological Noises
Not all knee noises are cause for concern. Physiological sounds often originate from harmless gas bubbles bursting in the joint fluid or ligament movement without pain. These noises typically require no treatment. Conversely, pathological noises are linked with cartilage wear, osteophytes, meniscal injuries, or instability and often accompany pain, swelling, or deformity. Recognizing these differences guides clinicians in recommending appropriate management or further investigations.
Nonsurgical Treatments: Managing Osteoarthritis and Knee Discomfort

What medical treatments are available for knee pain caused by osteoarthritis?
Medical treatments for osteoarthritis-related knee pain focus on reducing inflammation, relieving pain, and improving joint function. Commonly used medications include acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs help reduce inflammation and relieve pain by blocking enzymes that cause swelling, making them effective first-line treatments. When oral medications fall short, corticosteroid injections into the knee joint may be prescribed to provide targeted, temporary relief by decreasing inflammation directly within the joint. Another injectable treatment option is hyaluronic acid, which helps improve joint lubrication and reduces discomfort.
Physical therapy plays a vital role in nonsurgical management by strengthening muscles around the knee, improving flexibility, enhancing range of motion, and decreasing joint stress. Occupational therapy can also aid in teaching patients strategies to protect the knee during daily activities.
Lifestyle modifications complement medical treatments significantly. Weight management reduces extra stress on the knee joints, often resulting in less pain and slower disease progression. Regular, low-impact exercise such as swimming, cycling, or walking helps maintain joint mobility and muscle strength.
What role do medications like NSAIDs and corticosteroid injections play in treating osteoarthritis knee pain?
NSAIDs are powerful in mitigating inflammation and reducing pain symptoms associated with osteoarthritis by inhibiting enzymes responsible for producing inflammatory chemicals. Though effective, they are best used with caution over the long term due to potential side effects like gastrointestinal irritation or cardiovascular risks.
Corticosteroid injections provide focused relief when oral treatments and physical therapy are insufficient in controlling pain. By directly reducing joint inflammation, these injections often improve comfort and function temporarily. However, repeated corticosteroid use is generally limited to avoid possible cartilage damage.
Both NSAIDs and corticosteroid injections serve as important components alongside exercise, weight management, and other lifestyle changes in the comprehensive nonsurgical approach to managing knee osteoarthritis pain.
Additional pain relief methods and supportive care
Heat and ice application can help alleviate pain and stiffness. Using knee braces or supports may provide stability and reduce joint stress. Patients often benefit from education on activity modification to avoid movements that exacerbate symptoms.
Through a combination of medications, injections, physical therapies, lifestyle adjustments, and supportive care, many individuals successfully manage osteoarthritis symptoms without surgery.
| Treatment Method | Purpose | Additional Notes |
|---|---|---|
| NSAIDs | Reduce inflammation and pain | Effective but monitor long-term use side effects |
| Acetaminophen | Pain relief without anti-inflammatory effect | Suitable for mild to moderate pain |
| Corticosteroid injections | Targeted reduction of joint inflammation | Offers temporary relief; limited frequency advised |
| Hyaluronic acid injections | Improve joint lubrication | May reduce discomfort; evidence varies |
| Physical therapy | Strengthen muscles, improve mobility | Essential for functional improvement |
| Weight management | Decrease joint stress | Critical in slowing osteoarthritis progression |
| Pain relief methods (heat/ice) | Alleviate pain and stiffness | Simple adjunctive therapy |
| Bracing/support | Provide knee stability | Helps reduce joint stress and prevent injury |
The Power of Physical Therapy and Exercise in Knee Health
How effective are physical therapy and exercise in managing osteoarthritis-related knee pain?
Physical therapy and exercise play a crucial role in managing osteoarthritis (OA) of the knee. They are highly effective in reducing pain, improving joint flexibility, and enhancing muscle strength around the knee. Customized exercise programs typically include range-of-motion exercises to maintain or increase knee mobility, strengthening exercises to support joint stability, and neuromuscular training to improve balance and coordination.
Benefits of physical therapy for osteoarthritis
Physical therapy helps reduce inflammation and pain through techniques such as joint mobilization, which can also increase the range of motion in the affected knee. Moreover, it equips individuals with strategies to protect their joints during daily activities, thereby reducing stress and preventing further damage.
Exercise improving flexibility and strength
Regular exercise improves the flexibility of the knee ligament and tendons, making movements smoother and less painful. Strengthening the muscles around the knee, notably the quadriceps and hamstrings, provides better joint support and reduces the workload directly placed on the knee cartilage.
How strengthening prevents further joint damage
Stronger muscles absorb shock and stabilize the knee, which decreases wear and tear on the cartilage. This protective effect can slow the progression of osteoarthritis and lower the risk of future injuries related to joint instability or buckling.
Specific therapeutic techniques
Physical therapists employ various methods, including manual therapy, resistance training, aquatic therapy, and aerobic exercise, tailored to the individual's needs and capabilities. These techniques not only relieve pain but also enhance muscle performance and joint function.
Long-term outcomes and quality of life improvements
Sustained engagement in physical therapy and exercise programs has been shown to delay the need for surgical interventions such as knee replacement. Patients often experience improved mobility, reduced stiffness, and better quality of life. Additionally, maintaining an active lifestyle contributes to weight management, further alleviating stress on the knee joints.
In summary, physical therapy combined with regular exercise is a cornerstone in the comprehensive management of knee osteoarthritis. It effectively addresses symptoms and functional impairments, supporting long-term joint health and improved daily living.
When Is Knee Replacement Surgery Necessary?
When is knee replacement surgery recommended for osteoarthritis patients?
Knee replacement surgery is usually considered for osteoarthritis patients who experience persistent, severe pain and considerable functional limitations. These symptoms must not improve after at least six months of conservative treatments such as exercise programs, weight management, pain medications, and physical therapy.
What are the indications for knee replacement?
Surgery becomes necessary when osteoarthritis causes significant damage that restricts daily activities like walking, climbing stairs, and even sleeping due to pain. This level of symptom severity indicates that the knee joint is no longer functioning adequately to meet the patient's needs.
When do conservative treatments fail?
Conservative approaches aim to manage symptoms and improve function. However, if these methods fail to relieve pain or restore mobility over an extended period (typically six months or more), surgery may then be considered as the next step.
What factors influence decision-making for surgery?
Age, activity level, overall health, and lifestyle play crucial roles in deciding whether to proceed with knee replacement. Younger, more active individuals may delay surgery or consider alternative treatments, while older patients or those with disabling pain may benefit more immediately.
What are the risks and benefits of knee replacement?
Knee replacement generally results in significant pain reduction and improved quality of life for osteoarthritis patients. Yet, it involves risks such as infection, blood clots, and the need for revision surgeries later on. Hence, careful patient selection and thorough discussion between the patient and healthcare provider are essential to maximize success and minimize complications.
Emerging and Innovative Treatments for Knee Osteoarthritis
Are there any new or emerging treatments for managing knee osteoarthritis?
Knee osteoarthritis (OA) treatment is evolving with several innovative approaches gaining attention beyond traditional therapies. One promising advancement is genicular artery embolization, a minimally invasive procedure targeting abnormal blood vessels around the knee. By reducing blood flow to these vessels, the technique helps decrease inflammation and pain, offering relief without the need for major surgery.
Another breakthrough is the MISHA Knee System, an FDA-approved implantable shock absorber designed to redistribute mechanical stresses within the knee joint. This device acts as a cushion to reduce load on the damaged cartilage, potentially delaying the need for partial or total knee replacement surgeries, especially in younger or active patients.
Biologic therapies are also at the forefront of treatment research. These include platelet-rich plasma (PRP) and stem cell injections, which aim to harness the body's natural healing abilities. PRP uses concentrated growth factors from the patient's own blood to stimulate cartilage repair, while stem cells may regenerate damaged tissues and reduce inflammation. Although several studies report improvements in pain and function, their long-term benefits and ideal protocols remain the subject of ongoing clinical trials.
While these emerging treatments show considerable promise, healthcare providers emphasize the necessity for more rigorous research to fully understand their safety, efficacy, and best application scenarios. Patients considering these options should consult with specialized orthopedic or sports medicine professionals to tailor therapies appropriate to their individual condition and needs.
Looking Ahead: Caring for Your Knees
Popping knees without pain are usually harmless and part of normal joint function. However, persistent crepitus accompanied by pain, swelling, or instability may signal conditions like osteoarthritis or injury requiring medical evaluation. Advances in diagnosis and treatment, from conservative management to surgical options and emerging therapies, provide hope for maintaining knee health and mobility. Maintaining a healthy weight, regular exercise, and early consultation with healthcare providers are key to preserving knee function and enjoying an active life.
References
- Knee Noise: Crepitus and Popping Explained
- What Does a Pop in Your Knee Mean?
- Knee popping? You may be at risk for arthritis
- Why Do Knees Make Noise? - OrthoInfo - AAOS
- Knee Osteoarthritis: Symptoms, Stages, Causes & Treatment
- Why is My Knee Popping With Every Step | AKPC
- Noise around the Knee - PMC
- Why do your knees click and should you worry?